Submitted by Sophie Milbourne on Wed, 06/09/2023 - 12:50
Researchers from the MRC Toxicology Unit, in collaboration with the MRC Mitochondrial Biology Unit in Cambridge, have uncovered why individuals who are prescribed some antipsychotic drugs can develop movement disorders. How these side-effects might develop was not clear – until now - and it is all linked to damage to the mitochondria!
Schizophrenia is a complex neurological condition which usually involves symptoms of psychosis, or trouble distinguishing what is real from what is not in certain situations. It is thought that this is due to some brain cells sending too many dopamine signals. Dopamine is a neurotransmitter or a chemical messenger that allows brain cells to communicate. Fortunately, antipsychotic drugs can often be prescribed to help alleviate and prevent these symptoms.
A key type of antipsychotics are called dopamine antagonists. These are drugs that block dopamine, reducing the flow of messages between brain cells which can help to reduce psychotic symptoms.
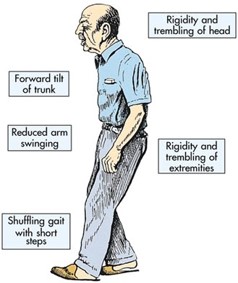
However, a significant minority of those prescribed these drugs (up to 15%) will develop debilitating movement disorders as a consequence, despite the drugs working therapeutically to improve their symptoms. This can cause many to stop taking these medications and no longer have pharmacological support for their symptoms.
The most recent so-called third generation antipsychotics act as dopamine partial agonists and were designed to reduce some of these negative side effects. They compete with dopamine to bind to the receptors on brain cells and keep dopamine signalling at a more controlled level. Unfortunately, this generation of antipsychotics still cause side-effects.
In order to reduce the number of individuals who develop these side-effects from antipsychotic medication, it is crucial to understand what is causing these side-effects to develop in the first place. To answer this question, the team led by researchers at the MRC Toxicology Unit explored whether third generation antipsychotics; aripiprazole, brexpiprazole and cariprazine, affected the function of the mitochondria and whether this might contribute to these side-effects.
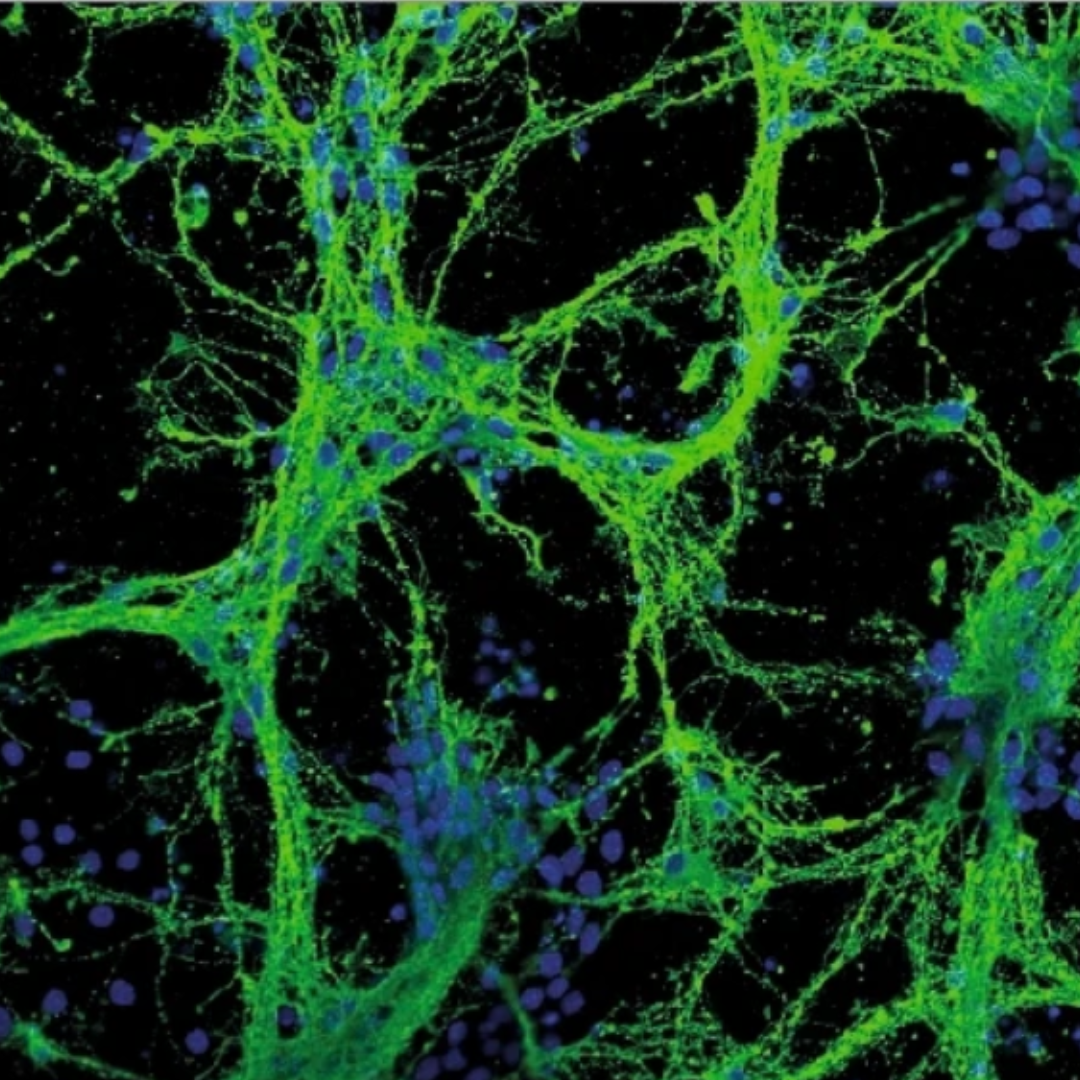
Mitochondrial respiration – the process by which our cells generate the energy they need – is vital for a wide range of physiological processes. When this process becomes dysfunctional, it can lead to several issues. For example, mitochondrial dysfunction is heavily implicated in neurodegenerative conditions.
By treating neurons with antipsychotics, they discovered that aripiprazole directly stops the electron transport chain (ETC) – a crucial series of chemical reactions that the mitochondria perform to generate the energy the cell needs.
The researchers also looked at the effects of these drugs in Drosophila melanogaster (fruit fly models). After 21 days of treatment with the drug, the flies displayed a decline in their mobility and, in parallel, the emergence of structural damage of mitochondria in the brain and muscle – without any damage to the muscle fibres themselves. These effects also got progressively worse after another seven days of treatment.
Whilst further study is needed to confirm that inhibiting the ETC in mitochondria directly causes the motor side-effects, this data supports clinical observations and shows a link between mitochondria and motor function when taking antipsychotics.
With this type of medication prescribed to millions globally, it is important to find treatment options that can reduce mitochondrial toxicity. This research could help to inform the development of antipsychotics that don’t inhibit the mitochondrial ETC and as a result decrease the incidence of these debilitating side-effects.
‘The antipsychotic medications aripiprazole, brexpiprazole and cariprazine are off-target respiratory chain complex I inhibitors’ was published on 1st August 2023 in the journal Biology Direct. Read the full publication here.